
Outer layer holes are more common and are often large with prominent rolled posterior borders. Inner layer holes are usually small and difficult to visualize.
The development of retinal holes in the inner and outer layers heralds a significant complication. Buch and colleagues reported a prevalence rate of 3.9% in those 60-80 years of age in Copenhagen, with a possible risk of increased retinoschisis progression in those receiving cataract surgery.

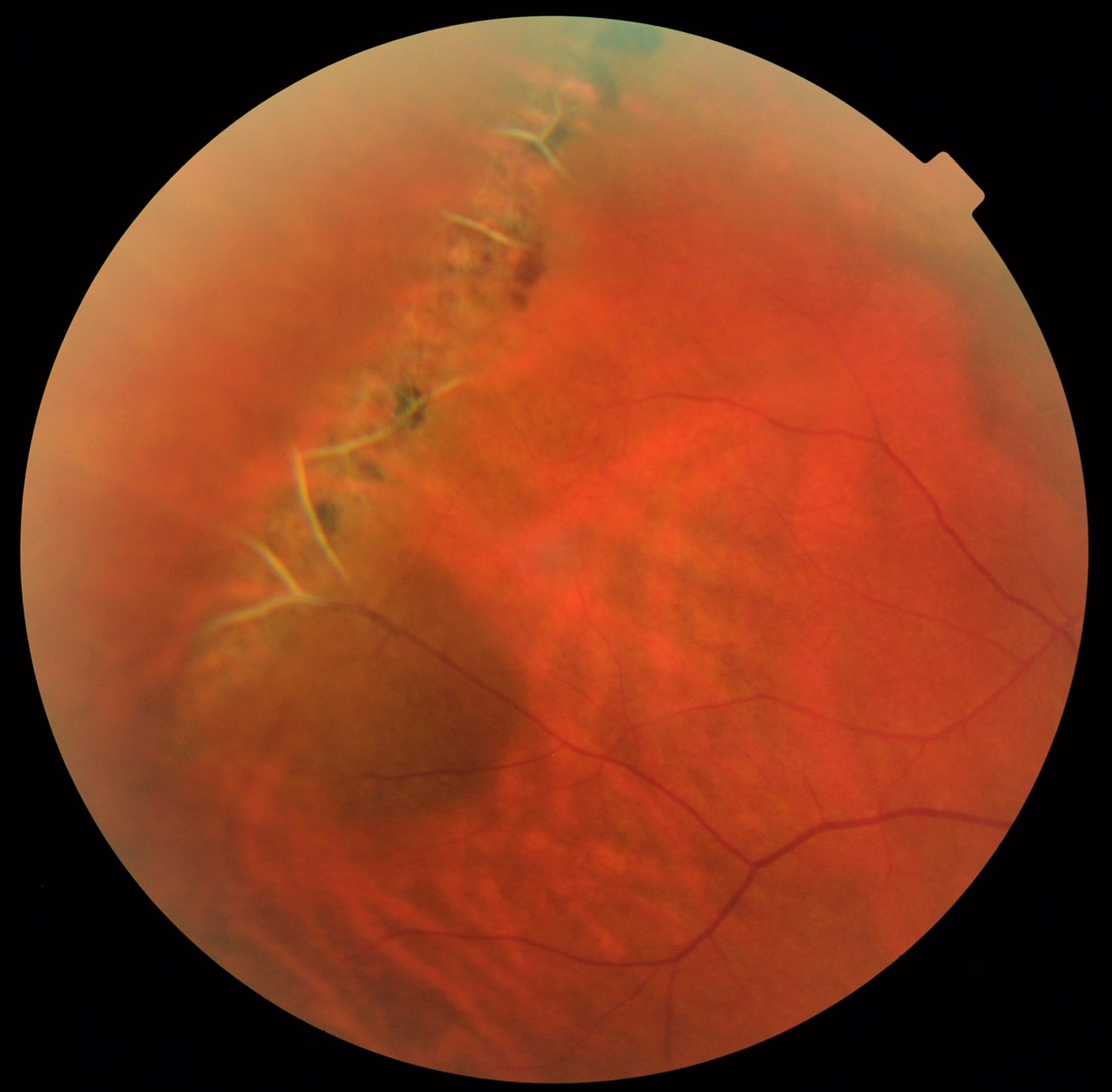
No cases of symptomatic progression occurred, but 14 cases of localized nonprogressive asymptomatic “schisis detachment” occurred. In the largest published series, Byer described the natural history of retinoschisis in 218 eyes studied for an average of 9.1 years4. Progression, when present, is slow, frequently stops spontaneously, and rarely reaches the macula. The natural history of retinoschisis in the absence of inner and outer wall breaks is typically benign, with uncommon, posterior extension. In contrast to retinal detachment, scleral indentation fails to collapse the cavity in retinoschisis. Scleral depression is essential in distinguishing retinoschisis from retinal detachment. If a pigmented demarcation line is present in the setting of retinoschisis, concomitant rhegmatogenous retinal detachment is present. Because the retinal pigment epithelium (RPE) is not disrupted by retinoschisis, hyperplasia does not occur and a demarcation line does not form. Whitish deposits, sometimes referred to as "snowflakes", and non-perfused, sclerotic retinal vessels can be found on the inner surface. The inner layer is often transparent and may be difficult to visualize. 3 Ophthalmoscopy reveals a smooth stationary elevation without folds and undulation upon eye movement. 2ĭegenerative retinoschisis is most commonly found in the inferotemporal quadrant. Eighty percent of the patients have bilateral involvement. Degenerative retinoschisis is idiopathic, and occurs equally in men and women with an incidence of 3.7% in patients 10 years or older and 7% in patients 40 years of age or older. This process results in the splitting of the retina at the outer plexiform layer and causes irreversible and complete loss of visual function in the affected area. 1 It develops as intraretinal microcysts located in an area of peripheral cystoid degeneration near the ora serrata coalesces. Degenerative retinoschisis was first reported by Bartels in 1933. Retinoschisis is notable for juvenile X-linked recessive retinoschisis and degenerative retinoschisis forms. Thus, our patient developed a rhegmatogenous retinal detachment as a result of inner and outer retinal hole formation in a retinoschisis cavity. The finding of a corrugated retinal appearance with outer retinal holes with an overlying intact inner retina is likely the result of rhegmatogenous detachment secondary to inner and outer wall retinal defects. However, degenerative conditions such as atrophic holes, lattice degeneration with atrophic holes, retinoschisis, and retinal tuft may also result in non-traumatic rhegmatogenous retinal detachment. These retinal detachments are seen in the setting of acute posterior vitreous detachment and lattice degeneration. Non-traumatic rhegmatogenous retinal detachment most commonly develops when a retinal break forms from vitreoretinal traction. A history of ocular blunt trauma should alert the clinician of the potential for retinal dialysis and giant retinal tear prompting peripheral examination with scleral depression. Traumatic rhegmatogenous detachment results from sudden compression-expansion injury of the globe with traction suddenly induced at the vitreous base, resulting in retinal dialysis or giant retinal tear. Even in the absence of a visible retinal break, this appearance as seen in our patient, is highly suspicious for rhegmatogenous detachment. Second is the corrugated appearance of the retina when detached.
#Retinal atrophic hole full
First, the finding of a full thickness retinal break in association with a retinal detachment is pathognomonic.

The diagnosis of rhegmatogenous detachment is characterized by two features. Exudative detachments are associated with retinal vascular, retinal pigment epithelial, or optic disc leakage resulting in dome-shaped detachments and the classically described “shifting” subretinal fluid. Traction-induced retinal detachments are seen in the setting of fibrovascular proliferative contraction with secondary retinal detachment. Retinal detachments are classified in four major categories tractional, exudative, rhegmatogenous, and combined traction-rhegmatogenous.


 0 kommentar(er)
0 kommentar(er)
